Abstract
Introduction: Daratumumab (DARA), a human IgG1k monoclonal antibody with single activity in multiple myeloma (MM) shows strong synergy in combination with other anti-MM agents, including immunomodulatory drug (IMiDs) and proteasome inhibitors (PI). This has led to the exploration of DARA in combination with front line regimens. Triplets including a PI and an IMiD are considered an ideal backbone with which to combine DARA prior to Autologous Stem Cell Transplantation (ASCT). However, based on the ability of Cyclophosphamide (Cy) to enhance DARA mediated antibody dependent cellular phagocytosis, we hypothesized that CyBorD may provide an alternative option (Naicker, ASH 2017). We are currently exploring the preliminary safety and efficacy of CyBorD and DARA as part of an ongoing phase 1b study in newly diagnosed MM (NDMM) pts eligible for ASCT. Last year we reported on the safety of this combination with an absence of dose limiting toxicity (DLT) with weekly subcutaneous (SQ) Bortezomib (Bor) 1.5mg/m2, Cy 300mg/m2 and DARA 16mg/kg (McEllistrim, ASH 2017). We now report on the efficacy of this regimen as pre-transplant induction, including the rate of CR post ASCT.
Methods: Pts received 4 cycles of induction therapy with weekly CyBorD and DARA 16mg/kg weekly for cycles 1 and 2 and every 2 weeks for cycles 3 and 4. Following induction therapy, pts proceeded to stem cell mobilization and ASCT followed by 2 cycles of consolidation therapy with weekly CyBorD plus DARA 16mg/kg on days 1 and 15. Following completion of consolidation therapy, all pts receive DARA maintenance every 28-days for 2 yrs or until progression, unacceptable toxicity or withdrawal of consent. Pts with high-risk features receive Bor on days 1 and 15 during maintenance phase. The primary endpoints were the incidence of DLT within the first cycle of combination at each dose level and CR rate post ASCT. Secondary endpoints included: safety, CR rate at the end of induction, consolidation and maintenance, best overall response, minimal residual disease (MRD) negative rate, progression-free survival, clinical benefit rate and overall survival. Responses were investigator-assessed as per IMWG criteria. This trial is registered at www.clinicaltrials.gov as NCT02955810.
Results: Eighteen pts were enrolled between Nov 2016 and Dec 2017 and received at least 1 dose of treatment. Baseline characteristics were: median age = 56 y (range 32-66); M (61%), F (39%), ISS stage I, II, III in 78%, 17% and 6% of pts, respectively. 28% patients were identified with high risk genetic features [17p deletion and/or t(4;14) by FISH and/or SKY92 (SkylineDx)]. Three patients discontinued therapy early (primary refractory, persistent liver toxicity, death, respectively).
Overall, treatment was well tolerated. The most common grade (gr) 3/4 hematologic treatment emergent adverse events (TEAE) were lymphopenia (44%), neutropenia (11%) and anemia (11%). The most common gr 3/4 non-hematologic TEAE were diarrhea (11%) and infection (61%). One patient died from gr 5 diffuse alveolar damage 7 weeks post ASCT. A single patient developed gr 3 liver toxicity. DARA-associated infusion reactions were ≤ gr 2 (11%).
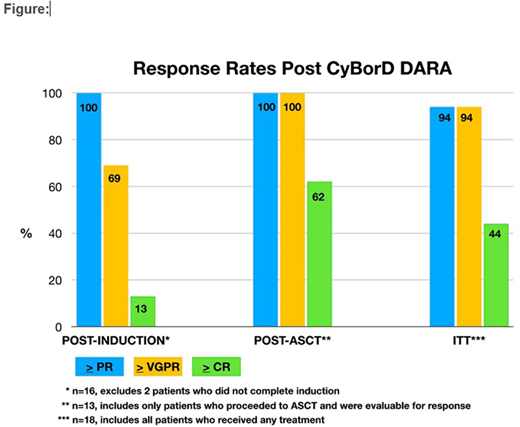
On an intent to treat (ITT) basis 94% achieved ≥ very good partial response (VGPR) with ≥ complete response (CR) in 44% pts (Figure). Among the sixteen patients completing 4 cycles of induction ORR was 100%, ≥ VGPR (69%), ≥ CR (13%). Informative NGS data (Adaptive Biotech) are available on 11/16 patients post induction, of whom 100% are MRD negative post induction at a level of ≥ 10e4. Following the induction phase 15/16 patients readily mobilized sufficient CD34 positive progenitors and proceeded to ASCT, one patient failed repeated mobilization. One patient died prior to post ASCT response assessment and data on the last patient is pending. Thus 13/15 patients are currently evaluable for response post ASCT. Responses deepened post ASCT with 100% achieving ≥ VGPR and 62% achieving ≥ CR. Based on EBMT criteria the CR/nCR rate post ASCT was 92%. Post ASCT PET-CT scans were consistent with complete metabolic response in all 13 patients. Updated results, including MRD status post ASCT will be presented at the meeting.
Conclusions: CyBorD-DARA is a highly active, well tolerated induction therapy for NDMM patients undergoing ASCT. These data support the further development of this combination as a convenient, cost effective alternative to PI-IMiD-DARA based combinations.
Quinn:Janssen: Honoraria. O'Dwyer:Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Research Funding; Glycomimetics: Research Funding; Onkimmune: Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Membership on an entity's Board of Directors or advisory committees; BMS: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal